In Vitro Fertilization (IVF) is an Assisted Reproductive Technique (ART) that fertility specialists use to help couples conceive babies. IVF clinics have produced millions of healthy “test tube babies” since 1988. In IVF, an egg or ova or multiple eggs or ova are removed from a woman’s ovaries, fertilized in a petri dish and returned to the woman’s uterus. This is different from surrogacy in which a woman unable to carry the fertilized egg in her uterus turns to a surrogate who carries the fertilized egg to full term.
In order to undergo an IVF procedure, a couple typically has to have trouble getting pregnant for at least one year through normal sexual intercourse. Problems conceiving can be caused by the male, the female, or both, and IVF procedures can help in whatever case.
The procedure typically costs from $5,000-$10,000 but can reach $25,000 if the procedure involves fertility drugs, attending multiple clinic appointments, and surgical procedures. The typical rate of success has improved from about 20% in 1995 to over 30% today.
One of the problems with in vitro fertilization, according to the Society for Assisted Reproductive Technology (SART), is the tendency for couples to have twins, triplets or more, born preterm or with risky low birth weights. This occurs because IVF specialists typically implant more than one egg to increase the chances of pregnancy, but this often leads to multiple pregnancies.
More Precise Identification of Healthy Embryos
One key factor in a successful IVF is choosing a healthy egg that results in a healthy and growing zygote or fertilized egg. Once an embryo is fertilized and placed back in the uterus, the current likelihood of a problem and the need for additional implants is from 20% to 35% with the best rates topping out at 40% for women with the best IVF profiles. An additional complicating factor is that many couples who seek IVF are over the age of 40, increasing the likelihood of unsuccessful IVF.
According to fertilization specialists, acupuncture procedures can help improve the likelihood of a successful outcome, as can fertility drugs.
EEVA Testing & Controversy
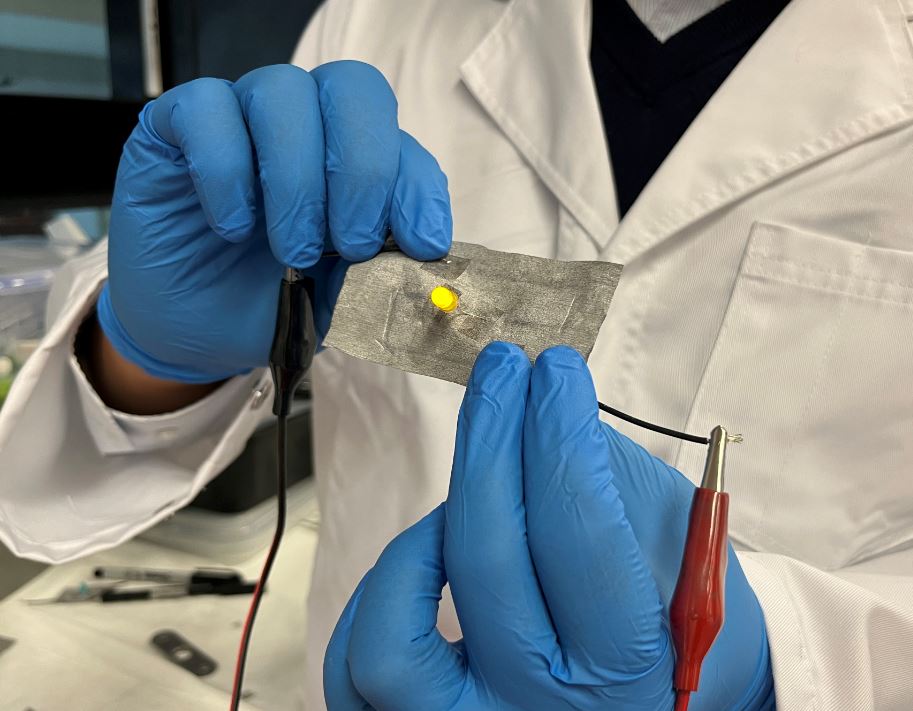
Barry Behr, director of the In Vitro Fertilization Laboratory at Stanford University, has created the Early Embryo Viability Assessment (EEVA) test to help determine which embryos are most likely to be most viable. The test is carried out after a typical day-three morphology test that assesses blastocyst formation. Embryologists in Europe have been using the test for about three years.
The EEVA test uses advanced software to analyze an embryo’s development, comparing it with clinically validated cell-division parameters using non-invasive measuring techniques instead of manual methods currently used in clinics.
References and related content: