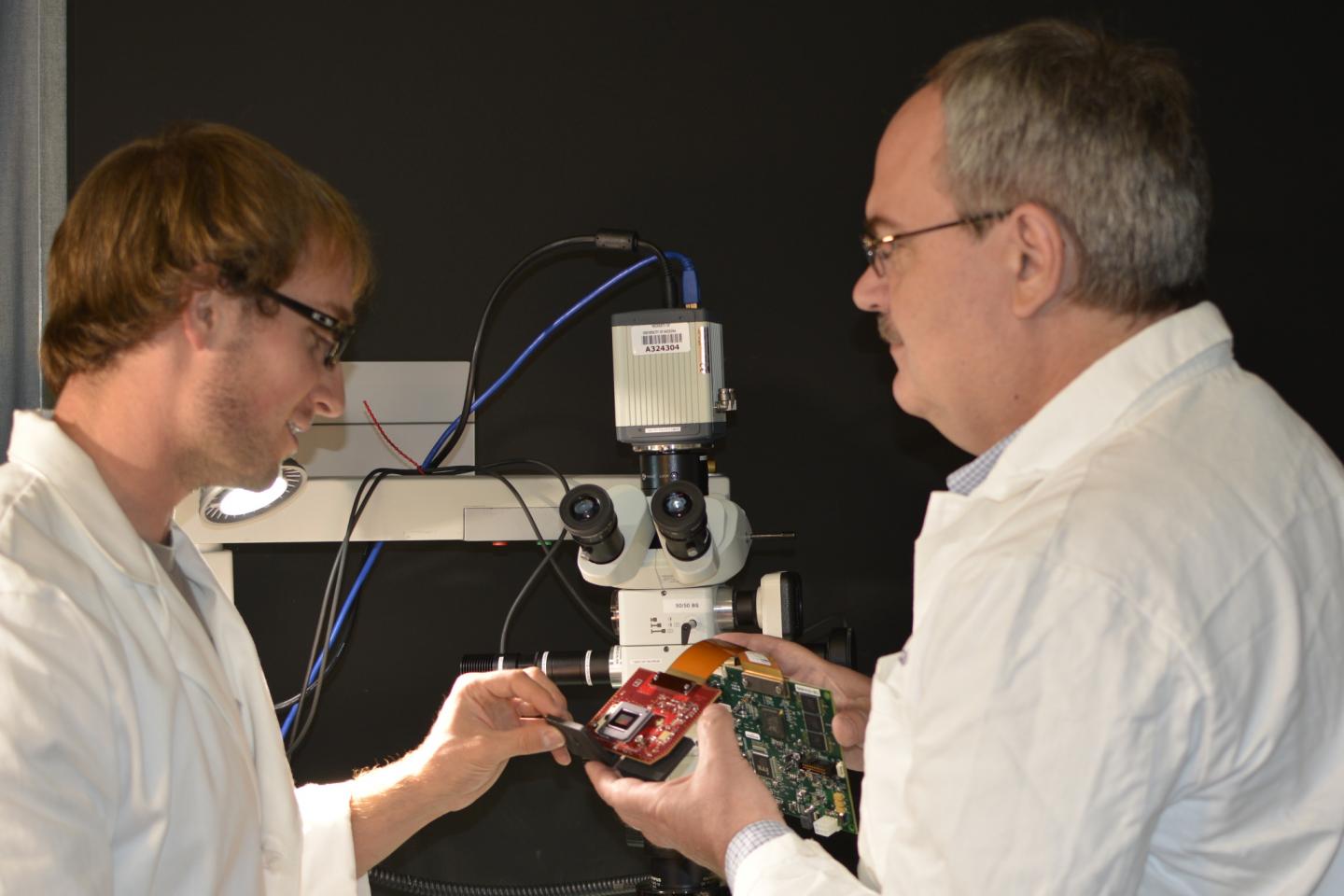
Bioengineers and neurosurgeons have collaborated to develop an enhanced microscopic technology that can assist surgeons in operating with augmented precision and decrease the risk of causing harm to patients.
The research team at the University of Arizona has invented an innovative machine that will, for the very first time, allow the surgeon to extensively utilize microscopes while operating, to observe blood flowing inside veins, and to differentiate between healthy and cancerous tissue by using a microscope.
The process is also known as augmented microscopy, which will produce a much more detailed picture for the surgeons to help them manage the surgery, where slight mistakes can cause paralysis, blindness, or worse, death.
Marek Romanowski, UA Associate Professor of Biomedical Engineering said in an interview, “When we started developing this technology, we thought of it like a Google map of a surgical view, providing layers of pertinent information in real time. Our augmented technology provides diagnostic information under the microscope on demand and in color, appearing directly over tissue a surgeon is operating on — as if the tissue was painted to help direct the surgeon’s work.”
The new technology generates a bright image that can be visualized by the surgeon under a microscope. The electronically enhanced image is processed by near infrared fluorescent lighting, which is a computer generated imaging technology, in which contrast agents are injected into the bodies of the patients to illuminate important diagnostic knowledge. This can help surgeons avoid cutting incorrect vessels or extracting healthy tissues.
However, the fluorescence only highlights black and white contrasts, not the structures or spatial relationships between different anatomical parts. So it will be the responsibility of the surgeon to correctly identify the lines of the anatomical structures. But it can prove to be crucial in avoiding interruptions and hesitation that can arise during guesswork regarding the location of a particular vein.
Jennifer Barton, interim director of the UA BIO5 Institute and a UA professor of biomedical engineering, specializes in cancer imaging. She said in an interview, “Surgeons need more information than can be provided by stereomicroscopes alone. Dr. Romanowski’s augmented microscopy technology provides critical functional information that can improve surgical accuracy and efficiency.”
Lemole, a former flight surgeon in the Air Force Reserve, compares the new technology to the head-up display system in the cockpit of a plane by saying, “If you can place your critical gauges directly in the pilot’s line of sight, they don’t need to look in a different direction while performing critical maneuvers. It won’t change the way they fly the plane, but it gives them more information, without distraction.”
The new technology is predicted to make headway in the brain surgery field by decreasing the risks associated with the process.