Antibiotics are becoming increasingly ineffective as bacteria have developed the ability to defeat the drugs designed to kill them.
This leaves doctors with fewer treatment options. The last-resort drugs kill the cells that are not targeted since the drugs randomly get distributed throughout our bodies. As a result, we often must take higher or repeated doses that heighten the risk of side effects.
Scientists have long been working on developing a targeted drug delivery platform to address the ongoing antibiotic resistance crisis
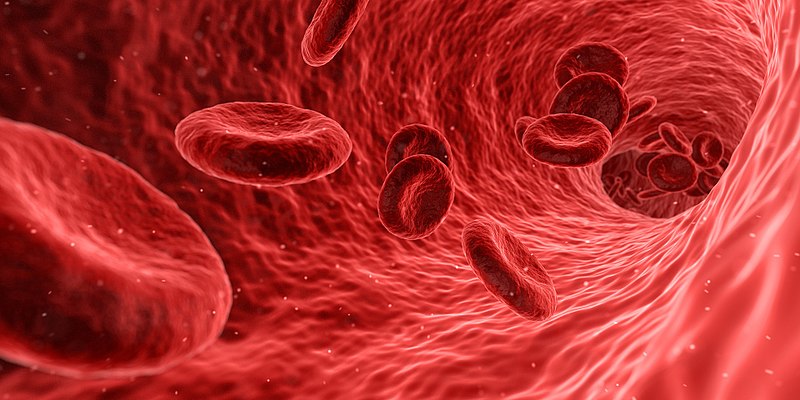
A new study by physicists at McMaster University has successfully modified the red blood cells to safely carry potent antibiotics to selectively target and kill bacteria. These smart red blood cells can carry antibiotics without interacting or harming healthy cells while passing through the body, potentially mitigating the side effects.
Researchers successfully developed a way to open the red cells to pull out the inner components and then load them with drugs instead. These hybrid blood cells are then injected back into the body to deliver the drug payload safely. To ensure that these hybrid blood cells reach the desired target, they coated the outside of the blood cells with antibodies which makes them stick to bacteria without the immune system attacking them.
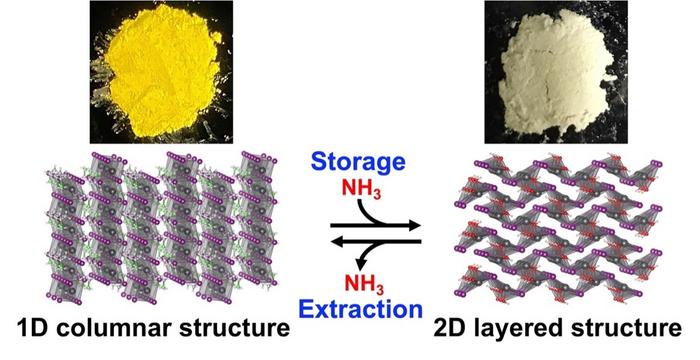
The researchers tested the drug delivery system with an antibiotic called Polymyxin B (PmB), which effectively kills drug-resistant bacteria. But this drug is considered a last-resort antibiotic since it has serious side effects.
The modified blood cells were loaded with PmB hybrid cells and coated with E. coli antibodies to target drug-resistant E. coli. It was found that the cells had a loading efficiency of around 90%, proving that selective targeting works. The technique could also reduce the number of doses and the number of drugs per dose.